Highmark wholecare prior authorization
October 1 — March 31, 8 a. Please note that a representative may contact you to confirm receipt highmark wholecare prior authorization information. By providing your email you will receive confirmation of your request as well as other helpful information from Highmark Wholecare. Enrollment in these plans depends on contract renewal.
Services centered around you. The services you need to keep your employees healthy. At MedExpress, we understand that accidents and illness can happen anytime. See the information below to help plan your visit to your MedExpress neighborhood medical center. Some exclusions may apply for select insurance plans. We strive to provide you with the best possible experience, including the insurance process.
Highmark wholecare prior authorization
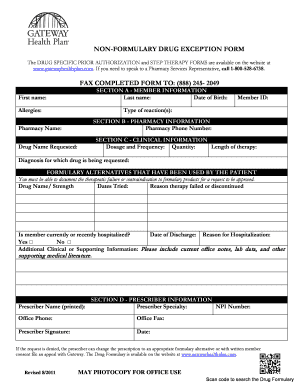
When considering medications from a class included on the Statewide PDL for MA beneficiaries, providers should try to utilize drugs that are designated as preferred. Drugs designated as non-preferred on the Statewide PDL remain available to MA beneficiaries when determined to be medically necessary through the prior authorization process. The Statewide PDL is a list of medications that are grouped into therapeutic classes based on how the drugs work or the disease states they are intended to treat. The committee's recommendations are approved by the secretary of the Department of Human Services DHS prior to implementation. The Statewide PDL is therapeutically based. The committee's recommendations are based on the clinical effectiveness, safety, outcomes, and unique indications of all drugs included in each PDL class. When drugs within a class are clinically equivalent, the committee considers the comparative cost-effectiveness of the drugs in the class. Back to Table of Contents. All non-preferred drugs on the Statewide PDL remain available to MA beneficiaries when found to be medically necessary. All drugs designated as non-preferred on the Statewide PDL require prior authorization through the beneficiary's pharmacy benefits provider. Some preferred drugs on the Statewide PDL require a clinical prior authorization. All preferred drugs that require clinical prior authorization remain available to MA beneficiaries when found to be medically necessary. All drugs designated as preferred with clinical prior authorization on the Statewide PDL require prior authorization through the beneficiary's pharmacy benefits provider. Prior authorization requests for beneficiaries who receive their pharmacy benefits through the Fee-for-Service delivery system should be directed to the DHS Pharmacy Services division.
Employer Services. Apply for Benefits. Need to Change Location?
This information will be used for purposes of performing services to, or on behalf of, our enterprise customers and prospective customers as part of and in relation to matters regarding our provider, health plan, and subsidiary enterprise care delivery, administration and operations. Your email address and phone number may be used to contact you. All reasonably appropriate measures will be taken to prevent disclosure of your Personal Data beyond the scope provided directly or indirectly herein or as may be reasonably inferred from the content contained in this notice or the website. Your Personal Data will be disclosed to appropriate personnel for purposes of performing services to, or on behalf of, our enterprise customers and prospective customers as part of and in relation to matters regarding our provider, health plan, and subsidiary enterprise care delivery, administration and operations. Notwithstanding the above disclosures, we will disclose the Personal Data we collect from you under the following circumstances:. We use third-party service providers to process Personal Data, including, without limitation, for information storage and other similar purposes. These services providers are located in the United States.
As a provider, you have access to a wide variety of tools and resources designed to help you deliver better service. If you haven't already done so, follow these simple steps to get the most out of your Highmark Wholecare partnership. Join our network by completing this form. Login to the provider portal. Review and download Medicare Assured and Medicaid Policies. Check out the Provider Newsletter. Highmark Wholecare participating providers have access to our Provider Authorization Portal.
Highmark wholecare prior authorization
Starting January 1, , Highmark Wholecare will no longer require prior authorization for over services. A listing of the affected Medicare and Medicaid services can be found on our website here. We value your continued partnership and hope this update will help add administrative efficiencies. If you have any questions, please reach out to your Provider Account Liaison.
Rooftop snipers unblocked
Plan Your Visit. You are now leaving a Highmark website. You can see a licensed MedExpress medical professional from the comfort of your home with secure video conferencing. Some preferred drugs on the Statewide PDL require a clinical prior authorization. Have Medicare and Medicaid? Highmark Wholecare serves a Medicaid plan to Blue Shield members in 13 counties in central Pennsylvania, as well as, to Blue Cross Blue Shield members in 14 counties in western Pennsylvania. This is not a valid zip code Required. All Medicaid covered drugs are available to beneficiaries when medically necessary regardless of the drugs' inclusion on the Statewide PDL. Telephone: For inquiries that cannot be handled via the online provider portal, call the appropriate Clinical Services number , which can be found here. Please view your local center page to view accepted insurance plans for your specific location. The Statewide PDL is a list of medications that are grouped into therapeutic classes based on how the drugs work or the disease states they are intended to treat. Get my kit. Medicaid-covered drugs in therapeutic classes that are not included in the Statewide PDL remain covered drugs for beneficiaries. We accept most insurances and offer convenient and affordable self-pay pricing for those without insurance. Manuals Highmark Provider Manual.
Introducing a new provider resource experience that simplifies getting you the information you need, when you need it. Your feedback is appreciated as we work to complete the experience. The authorization is typically obtained by the ordering provider.
Your free Highmark Wholecare Enrollment Kit will include:. Additional Resource: MCG Guidelines Product Acronym List Fax: If you are unable to use the online provider portal, you may also fax your authorization requests to one of the following departments. Get my kit. Services centered around you. For additional information regarding your specific plan and coverage, please contact your insurance provider directly. Some preferred drugs on the Statewide PDL require a clinical prior authorization. Please enable scripts and reload this page. Please zoom in closer or click on a pin to view information about a specific MedExpress center. Benefit plans vary widely and are subject to change based on the contract effective dates. Effective dates are subject to change. Highmark Wholecare serves a Medicaid plan to Blue Shield members in 13 counties in central Pennsylvania, as well as, to Blue Cross Blue Shield members in 14 counties in western Pennsylvania. Highmark will provide written notice when codes are added to the list; deletions are announced via online publication.

I consider, that you commit an error. Write to me in PM, we will discuss.