Postpartum hemorrhage ati
Federal government websites often end in.
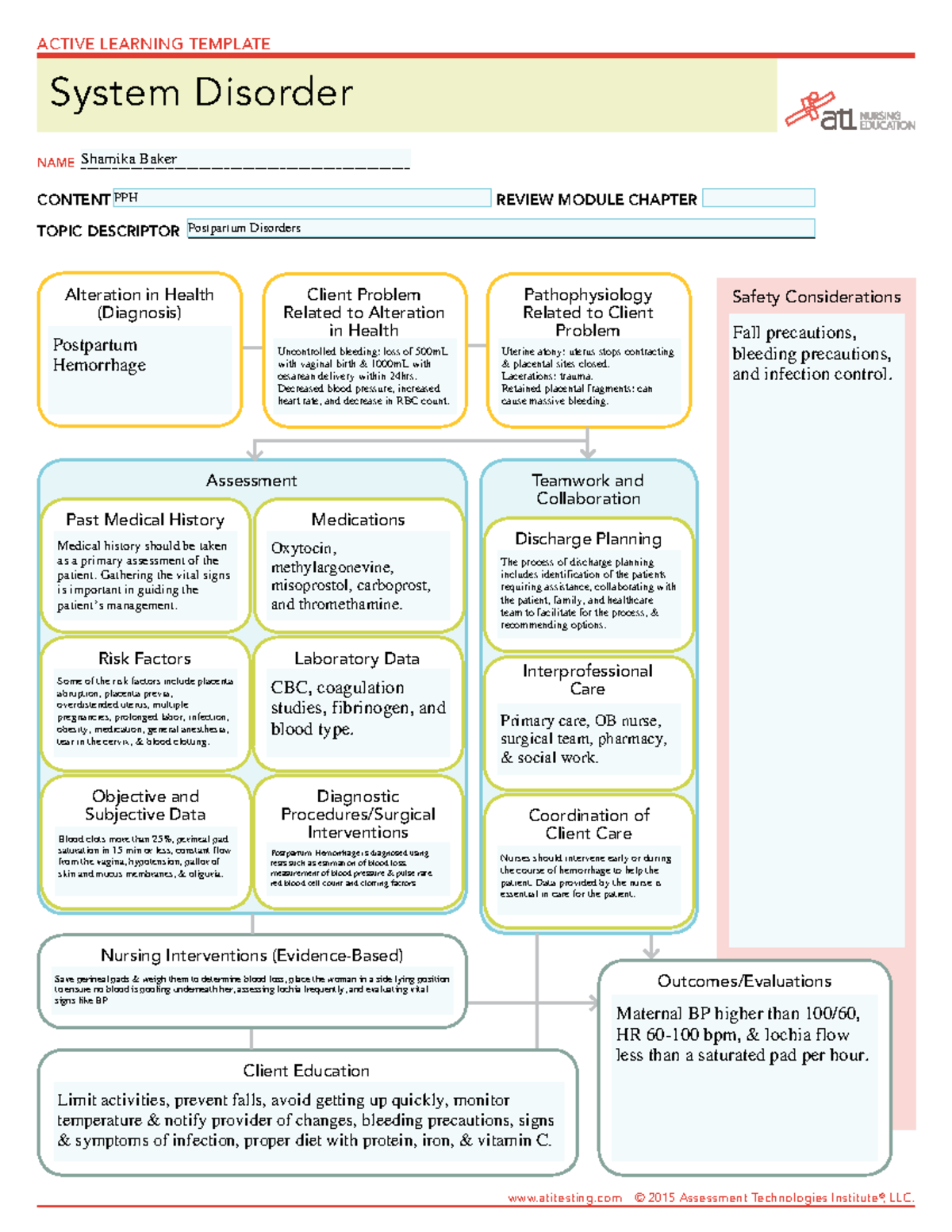
The postpartum period, a time of joy and celebration, can also present unexpected challenges, one of which is postpartum hemorrhage PPH. It accounts for the majority of the 14 million cases that occur each year. Postpartum hemorrhage is a significant and potentially life-threatening complication that requires prompt recognition, rapid intervention, and expert nursing care to ensure the well-being of the mother. As nursing professionals, understanding the risk factors, early signs, and evidence-based interventions for PPH is crucial in providing comprehensive care and support during this critical phase of the maternal journey. This article aims to serve as a comprehensive nursing guide to postpartum hemorrhage , delving into its causes, assessment techniques, and multidisciplinary management.
Postpartum hemorrhage ati
.
You are not required to obtain permission to distribute this article, postpartum hemorrhage ati, provided that you credit the author and journal. Postpartum hemorrhage is a leading cause of maternal and fetal morbidity in the United States. Vascular ligation sutures may be attempted to decrease pulse pressure at the uterus.
.
Federal government websites often end in. Before sharing sensitive information, make sure you're on a federal government site. The site is secure. NCBI Bookshelf. Kelly C. Wormer ; Radia T. Jamil ; Suzanne B. Authors Kelly C.
Postpartum hemorrhage ati
Complications of postpartum hemorrhage are listed in Table 1 3 , 6 , 7 ; these range from worsening of common postpartum symptoms such as fatigue and depressed mood, to death from cardiovascular collapse. This review presents evidence-based recommendations for the prevention of and appropriate response to postpartum hemorrhage and is intended for physicians who provide antenatal, intrapartum, and postpartum care. Risk factors for postpartum hemorrhage are listed in Table 2. The most effective strategy to prevent postpartum hemorrhage is active management of the third stage of labor AMTSL. AMTSL also reduces the risk of a postpartum maternal hemoglobin level lower than 9 g per dL 90 g per L and the need for manual removal of the placenta. Based on existing evidence, the most important component is administration of a uterotonic drug, preferably oxytocin. An alternative to oxytocin is misoprostol Cytotec , an inexpensive medication that does not require injection and is more effective than placebo in preventing postpartum hemorrhage. The benefits of controlled cord traction and uterine massage in preventing postpartum hemorrhage are less clear, but these strategies may be helpful. Diagnosis of postpartum hemorrhage begins with recognition of excessive bleeding and targeted examination to determine its cause Figure 1 6.
Bulls 91
Conditions that could have caused cervical or uterine lacerations. Objectives: Identify the etiology of postpartum hemorrhage. Access free multiple choice questions on this topic. Wormer 1 ; Radia T. Consultations An interprofessional approach is mandatory for the required outcomes in the management of a patient suffering from acute postpartum hemorrhage. Authors Kelly C. Similar articles in PubMed. If bimanual massage and uterotonic medications are not sufficient to control hemorrhage, uterine tamponade may be considered. Careful direct assessment of cumulative blood loss is important, and a focus should be on the early initiation of protocols for the release of blood products and massive transfusion protocols. A woman who underwent operative birth or rapid birth could develop lacerations that would cause bleeding. The site is secure. The complications related to management include the following: Transfusion-related acute lung injury. As nursing professionals, understanding the risk factors, early signs, and evidence-based interventions for PPH is crucial in providing comprehensive care and support during this critical phase of the maternal journey. Primary causes of postpartum hemorrhage include:. Search for:.
The postpartum period, a time of joy and celebration, can also present unexpected challenges, one of which is postpartum hemorrhage PPH.
Int J Gynaecol Obstet. The treatment and management of postpartum hemorrhage are focused on resuscitation of the patient while identifying and treating the specific cause. Primary causes of postpartum hemorrhage include:. Antifibrinolytic drugs for treating primary postpartum haemorrhage. Acute Postpartum Hemorrhage. Review Active management of the third stage of labour: prevention and treatment of postpartum hemorrhage. The best events are yet to come, but the safety and health of both the mother and the baby should still be monitored. The postpartum period, a time of joy and celebration, can also present unexpected challenges, one of which is postpartum hemorrhage PPH. Nurses also need to intervene early or during the course of a hemorrhage to help the patient regain her strength and vitality. Bleeding of more than mL in a normal vaginal delivery and more than mL in a cesarean birth qualifies for a postpartum hemorrhage.

0 thoughts on “Postpartum hemorrhage ati”